Mohs Surgery
Mohs micrographic surgery is a specialized, highly effective technique for the removal of skin cancer. The procedure was developed in the 1930s by Dr. Frederic Mohs at the University of Wisconsin and is now practiced throughout the world. Mohs surgery differs from other skin cancer treatments in that it permits the immediate and complete microscopic examination of the removed cancerous tissue, so that all “roots” and extensions of the cancer can be eliminated. Due to the methodical manner in which tissue is removed and examined, Mohs surgery has been recognized as the skin cancer treatment with the highest reported cure rate.
What skin cancers are treated with Mohs surgery?
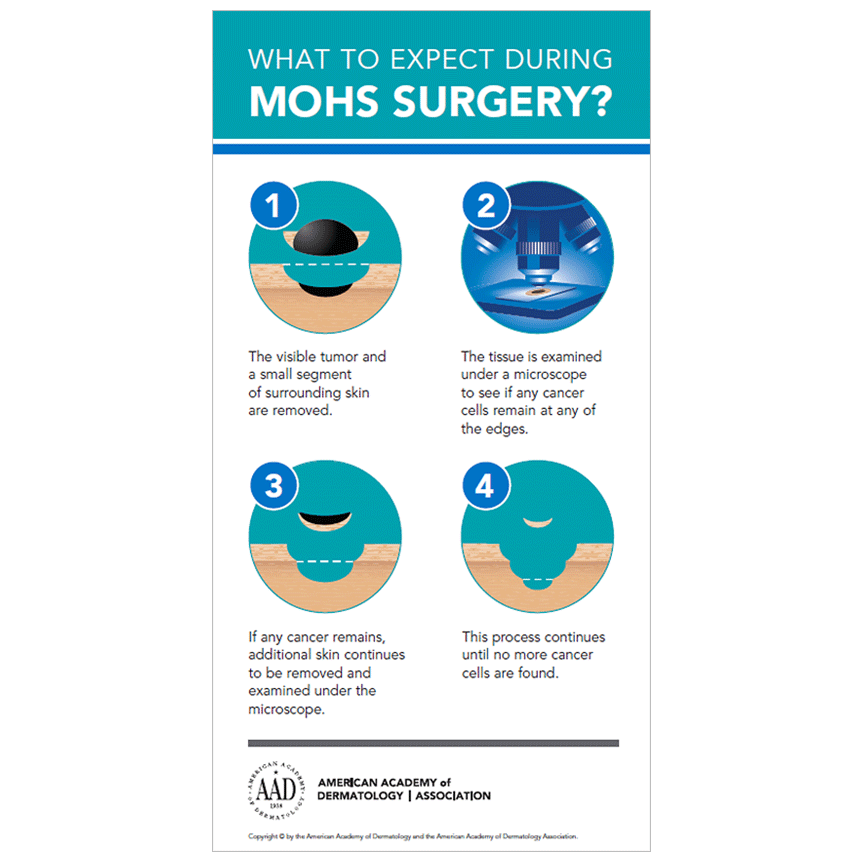
The Mohs Surgeon performs the dual role of skin cancer surgeon and pathologist. The Mohs procedure involves the surgical removal of the visible portion of the skin cancer, along with a layer of the surrounding skin. This tissue is then divided into sections and color-coded by the Mohs surgeon, while corresponding reference marks are made on the patient to indicate the source from which each section was taken. The surgeon then draws a map of the surgical site, and the tissue is processed to create microscope slides for examination and analysis by the physician. He or she then examines the undersides and edges of each section microscopically for evidence of remaining cancer cells. If cancer is still present, the involved areas are carefully marked on the map and the patient is prepared to undergo removal of another layer of tissue. It is important to note that any additional tissue is removed only from the area(s) in which cancer cells are still evident on microscopic examination. This process is repeated until no further evidence of cancer remains at the surgical site. The repair is then performed by the Mohs Surgeon.
Mohs surgery can be described as the surgical removal of skin cancer and other appropriately indicated malignancies followed by microscopic examination of graphically oriented, oblique tangential histologic sections of the entire surgical margin of excised tissue, to ensure the complete removal of the malignant tissue.
How Effective is Mohs Surgery
Clinical studies have demonstrated that Mohs surgery provides five-year cure rates approaching 99% for new cancers and 95% for recurrent cancers. Important advantages of the Mohs procedure are that it allows the greatest amount of surrounding healthy tissue to remain intact, potentially reducing the size of the final surgical defect and resulting scar. The methodical manner in which all lateral and deep tissue margins are examined enables the surgeon to detect and remove any “roots” of the skin cancer that may be present, which greatly reduces the likelihood of recurrence.
Who is Mohs recommended for?
No matter what type of skin cancer you have, Mohs is only recommended for certain patients. The AAD and ASMS recommends Mohs surgery on skin cancers that:
- Develop on cosmetically sensitive areas (i.e. face)
- Are located in scar tissue
- Are large and/or have ill-defined borders
- Develop on areas that need to retain function (i.e. eyelids)
- Have recurred after previous treatment or are likely to recur
- Grow rapidly
- Multiple skin cancers that are very close together
*The above Mohs surgery information has been provided by the American Academy of Dermatology.
